
Constipation and Pelvic Floor Dysfunction - What You Need to Know Postpartum

If you just had a baby you are likely talking about poop way more than you ever have in your whole life (ok maybe with the exception of healthcare workers.) You are focused on the size, the color, the frequency, the blow outs. Oh the blow outs!
While you maybe hyper focused on your little ones BM habits – and with good reason, they can tell you a lot, you are probably neglecting your own bowel habits.
Constipation is a common but not usually discussed topic postpartum. It usually only last the first few days but can last 3-6 months. For some it persists up to a year after birthing their baby. While constipation is common with all deliveries it is even more common if you had a caesarean birth. This is due to the use of anesthesia and pain medications
What is constipation
Constipation is difficulty passing stool and/ or having three or fewer bowel movements in a week. Stool might be hard and segmented, require straining to pass, be accompanied by pain or discomfort or feel as though you didn’t empty completely.
Generally constipation isn’t a serious threat however it can greatly impact your comfort and quality of life and can significantly impact your pelvic health and recovery. These are issue enough to take notice and take action.
While constipation usually isn’t threatening there are times it could be more emergent. If you haven’t had a bowel movement in over a week, if you have alternating bouts of constipation and diarrhea, constipation with severe abdominal pain or bloody stool you want to call your doctor right away.
Constipation and your pelvic floor
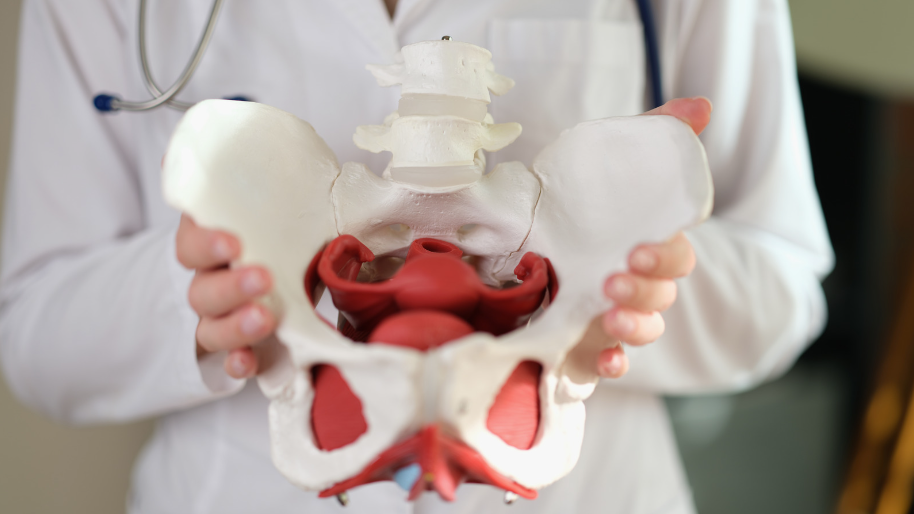
There is correlation between pelvic floor issues and constipation. The two can beget each other. Chronic constipation can cause pelvic floor issues and pelvic floor issues can cause constipation. For better pelvic health you want to do your best to avoid constipation.
If your rectum (the last portion of your large intestines that connects your colon and anus) isn’t able to empty that can place consistent pressure on your pelvic floor. Overtime this can weaken the pelvic floor muscles. As stool is unable to pass it can also put pressure on the bladder and urethra which can lead to incontinence or frequency issues. If you are having to strain with your bowel movements that can further cause pelvic floor dysfunction.
Pelvic floor dysfunction can also cause constipation if there is too much tension in the muscles, they are unable to lengthen and relax your stool may be prevented from passing. This causes straining which only further leads to muscle tightness and dysfunction. Prolapse especially a rectocele (when the back portion of the vagina bulges into the rectum) can also cause constipation. With a rectocele it is often difficult to have a complete bowel movement as pieces of stool get stuck in the bulge that is created.
Your first postpartum bowel movement

It is not uncommon to be fearful of having your first bowel movement after baby. Depending on how open you are with your friends and family this is either something you have heard horror stories about or radio silence. In my opinion neither is super helpful. What you need is to be prepared and have some practical tips to make it more easeful and yes less scary.
Typically it can take 3-4 days after having your baby to have your first bowel movement. Of course for some they may have a BM the next day and for others it can be up to 5 days. If you are nearing a week without a bowel movement, call your doctor.
Keep in mind that your body is still processing the birth and going through some major changes that can affect your bowel movements. Increased uterine contractions as your uterus returns to size could cause looser stool than usual. Increased stress hormones can lead to increased constipation or looser stool depending on how your individual body reacts. So expect some changes.
If you used to be very regular chances are you have no semblance of a routine at the moment and this can also impact your daily bowel movement habits.
If you had a vaginal delivery the thought of passing anything else (even just a bowel movement) can seem terrifying. You need time to process. If you had a c-section you maybe experiencing abdominal pain and discomfort.
Hygiene after your first bowel movement
Once you do finally have your first bowel movement it is important that you avoid wiping. This can cause irritation to your already tender tissue and can disrupt any healing or stitches if you had tearing or an episiotomy. You can dap with paper and otherwise you will want to use a peri bottle. There is no strict rule for how long you should use a peri bottle but at least 1 week is a good place to start. You want to continue to use the peri bottle as long as you are tender and sore. When you do return to wiping you want to make sure you go from front to back to decrease chance of a urinary tract infection.
Tips to ease constipation for better pelvic health
Follow these tips if you are getting ready for your first postpartum poop or you are several weeks or months out and experiencing postpartum constipation.
Brace your incision
You can feel more pressure and discomfort over your incision. This is true for a caesarean birth and also if you had vaginal tearing or an episiotomy. If you had a caesarean birth you can cross your arms over your incision or hold a pillow over the area as you lean forward slightly while you have your bowel movement. For vaginal incisions or tears use a clean pad or some toilet paper and gentle press over the area as you have a bowel movement.
Drink plenty of water

Your intestines pull out water when you are dehydrated. This makes stool harder in texture and more difficult to pass. Generally you want to drink 8-10 glasses of water a day. If you are breastfeeding you will need to increase this by 4-6 glasses of water a day as breastmilk uses a lot of your water supply.
Fiber

Dietary fiber is important for quality stool. The Mayo clinic explains how fiber helps add bulk and softness to your stool making it easier to pass. It is recommended to eat 28-30 grams of fiber a day. However this is a generalization, check with your dietitian or physician if questions or concerns. As you add in fiber you will want to do so gradually to avoid cramping and bloating. While there are supplements available try to eat most of your fiber from food such as whole grains, nuts, legumes, berries and vegetables.
Pre and probiotics
Speaking of eating your fiber it is also important to eat your pre and probiotics. Pre and probiotics are shown to improve and maintain a healthy gut microbiome and it is noted that a healthy gut is needed for regular, healthy bowel movements. Supplements can be helpful but eating pre-and probiotics can give you a bigger bang for your buck. Supplements tend to be expensive and fermented foods are shown to be a great source of probiotics. Fermented such as pickles, kimchi kombucha, miso, apple cider vinegar, yogurt are all great choices. Try adding one serving of fermented food into your daily diet.
Movement

Your gastrointestinal (GI) tract is motile, it requires movement to move the food along to create stool and ultimately a bowel movement. If you are not moving, your gut is not moving. Early in postpartum our typical movement levels tend to decrease drastically as we are healing and adjusting to new mom life and also our sleep (or lack there of) routine. Walking is one of the best activities you can do early in postpartum you can start with a few laps around your house and work up gradually to 10 and then eventually 30 minutes walks.
Need a little guidance on how to ease into gentle movement during the first 6 weeks, Grab Your Postpartum Plan Here!
Process your birth story and seek postpartum support
When we are stressed we go from a parasympathetic to sympathetic state in our nervous system. This moves blood flow from our gut when we are in our parasympathetic (rest and digest) state to our limbs as we go into our sympathetic (fight/flight) state. If we are in a constant level of stress for a long time if can affect our GI system, slowing it down and eventually lead to constipation. Of course for some they may experience loose stool in stressful situations but this is usually acute situations. Chronic stress tends to cause more constipation as GI motility slows down, blood flow is decreased to the area and sometimes chronic stress can lead to abdominal pain which can cause constipation.
Our bodies hold onto stress and tension in our muscles. Our pelvic floor is a very common area to hold onto this tension. Birth can be traumatic, even when it goes well. Our bodies hold onto that trauma as stress and muscle tension.
Processing your birth story and seeking support during your postpartum can help. Not only can it decrease muscle tension but help improve mood and your ability to function throughout the day.
GI massage
GI massage can improve peristalsis by triggering the contractions in the intestines. Start on your back and bring both knees into your chest. Hold for 1-2 mins and gently rock side to side and back and fourth.
You can also trace your hands along your large intestines using firm but gentle pressure and long strokes. Start at your right lower abdomen just inside the top of your pelvis, go up until you reach your rib cage, go straight across the top of your abdomen until about nipple line, then go down until you hit your pelvis, move to the center across your lower abdomen until you are at your midline in line with your belly button and then go down towards your pubic bone. Do this on repeat for 2-3 minutes either on your back or left side lying.
If you are within your first 6 weeks and had a c-section, be mindful of your incision. Skip over the incision line during that time. After 6 weeks you can go right over it.
Stool softeners
If you are very early postpartum, within your first few weeks, you were likely given or prescribed stool softeners. Take them! Take them for the first full week home. After that you can most likely stop taking them. If you are experience constipation after that point you may need to resume them. If you were also prescribed iron you will want to take them throughout the duration of the iron supplementation. Of course discuss with you physician if any questions.
How you go to the bathroom matters
Your position matters. You want to have your knees above your hips for optimal positioning with having a bowel movement. This position improves the position of your rectum and also allows for improved pelvic floor length and relaxation. You can use a squatty potty or any step stool you have will work fine.

Looking for more support early postpartum?
Struggling with postpartum pelvic pain, leaks, or discomfort? Download your FREE Postpartum Pelvic Recovery Guide and learn simple, expert-backed strategies to heal, strengthen, and feel like yourself again. Because your recovery matters—let’s take care down there!
Thank you for sharing!
